Recognizing the signs early is key
Considering that pets cannot communicate when their medical condition is getting worse, being able to recognize signs that a pet is deteriorating is critical to your pet’s successful treatment and well-being.
This is especially true with medical conditions that lead to hypoxemia (a lack of oxygen in the blood) as this can quickly become a potentially life-threatening emergency.
There are many conditions that can lead to hypoxemia like Collapsing Trachea, CHF, and Feline Asthma – these are all common veterinary conditions that are managed at home, but will likely recur or progress, resulting in hypoxemia and respiratory distress.
3 things to check to check your pet for:
1. Listen for airway noises
Pets should not be making a lot of noise while breathing. A honking noise, stridor (high-pitched continuous squeal usually on inspiration, or breathing in), or stertor (discontinuous low-pitched sounds like clicking or snoring) heard from a dog with collapsing trachea, laryngeal paralysis, or brachycephalic syndrome, may indicate that the pet is having trouble getting air in or out.
Likewise, wheezes heard from a cat may also indicate respiratory distress. It is important to know what normal sounds your pet makes when they are breathing, as these respiratory noises can be the first clue that a pet is starting to decompensate and needs help breathing.
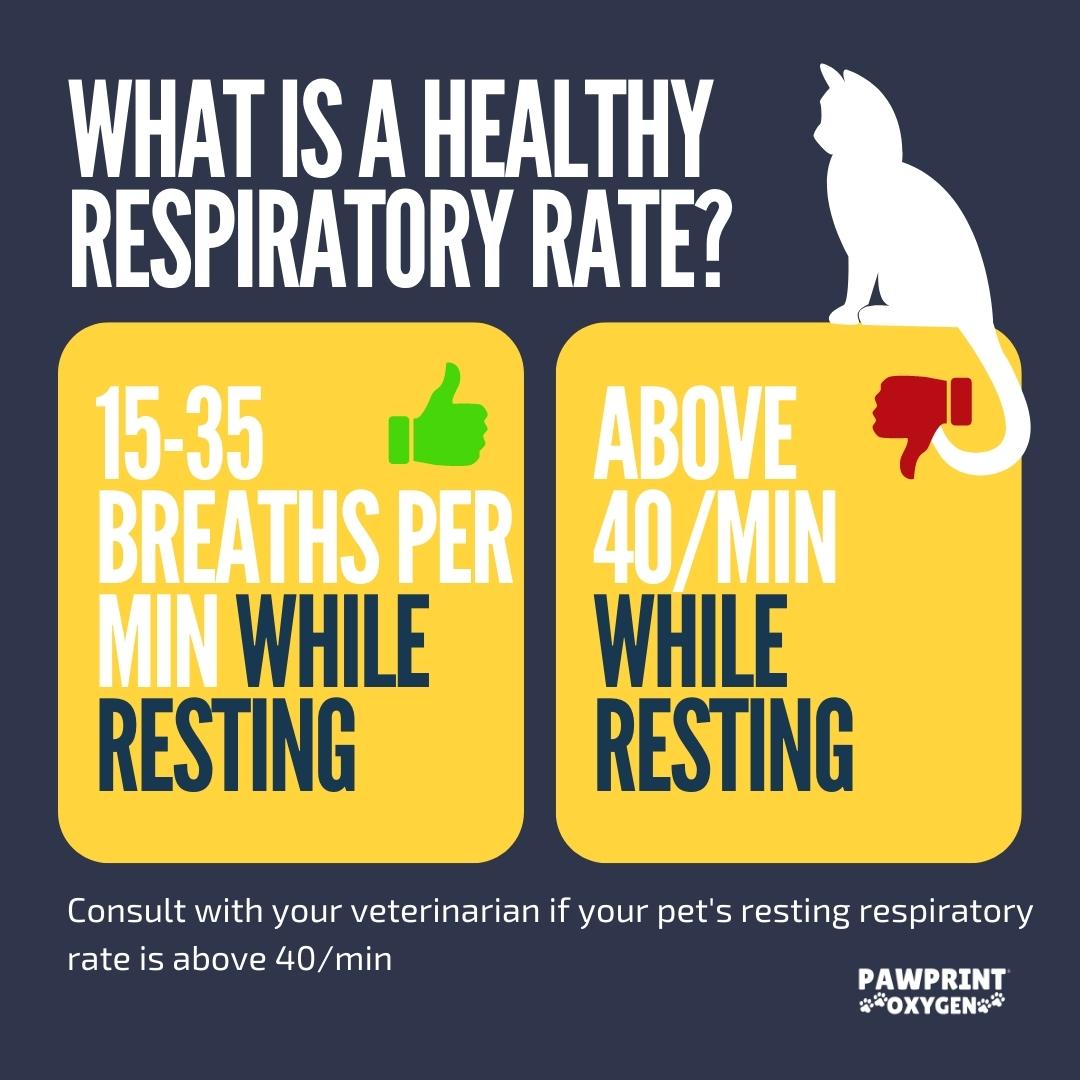
2. Assess your pet’s Respiratory Rate and effort
After listening for airway sounds, assess the breathing for both rate and effort. This will (if nothing else) provide a starting point for you to monitor your pet’s respiratory rate going forward.
Normal rates of respirations in a pet are up to 40 breaths /minute. To assess the rate of respiration, count the number of breaths in 15 seconds, then multiply this value by 4. For example, a cat who takes 8 breaths in 15 seconds has a respiratory rate of 32. The low end of respiratory rate is only relevant if the pet has a disease or condition that can cause slow breathing, and while the cut-off value for slow breathing is technically 20 breaths/minute, it can be as low as 12 breaths/minute in a deep sleeping pet. On the high rate end, panting dogs confound this evaluation even for veterinarians, so knowing your pet and their breathing rate after excitement or activity is imperative.
Just as, if not more important than the respiratory rate is respiratory effort. Again, to know what is abnormal, one needs to know their pet’s normal respiratory effort including after some activity and excitement.
One looks at the chest—how much the chest moves in and out along with abdominal effort. Pets usually do not recruit their abdominal muscles to help them breathe unless they have just exerted or are trying to cool themselves. Deeply exaggerated chest excursions or shallow frequent breaths (in the absence of panting) are also clues that the pet may be hypoxemic.
Another sign of increased respiratory effort is open-mouth breathing. Cats breathing with their mouth open is always a concerning sign. The same is true for dogs that are not heat-stressed or have just exerted themselves. Additionally, dogs standing with extended necks flared nostrils, and elbows out are working very hard to breathe.
3. Check for blue gums or tongue
One should not shove anything into or near the mouth of your pet to avoid getting bit or impeding your pet’s breathing; however, if a pet’s tongue or gums have a blue tint, referred to as being “cyanotic,” the pet is indeed hypoxemic and experiencing respiratory distress.
Unfortunately, a pet with pink gums and tongue is not necessarily normal so one has to infer based on the pet’s other signs to determine if they are showing signs of respiratory distress.
Talk to Your Veterinarian
A pet in respiratory distress is a medical emergency and an action plan that has been pre-determined with a veterinarian should be instituted when signs indicate that the pet’s condition has deteriorated.
Speak to your veterinarian today about having on hand in case your pet is having a respiratory emergency at home and requires transport to a veterinary practice.
Oxygen Kit for Dogs
Get your pet to the hospital safely during a respiratory distress event with Pawprint Oxygen’s transport kit or administer at home to safe a trip to the veterinarian
Oxygen Kit for Cats
Get your pet to the hospital safely during a respiratory distress event with Pawprint Oxygen’s transport kit or administer at home to safe a trip to the veterinarian
About Sean Smarick, VMD, DACVECC

Dr. Sean Smarick received his Doctor of Veterinary Medicine from the University of Pennsylvania in 1991. He then completed a residency in Veterinary Small Animal Emergency and Critical Care at the University of California, Davis in 2003 and, in the same year, became a Diplomat of the American College of Veterinary Emergency and Critical Care. In his 30 years of practice, Dr Smarick has enjoyed being in the ICU and emergency rooms of private and university practices, participating in CPR and clinical research, contributing to journals and textbooks, training residents and interns, and serving on the board of several veterinary businesses and organizations.